
MENISCUS TEARS: SURGICAL TREATMENT
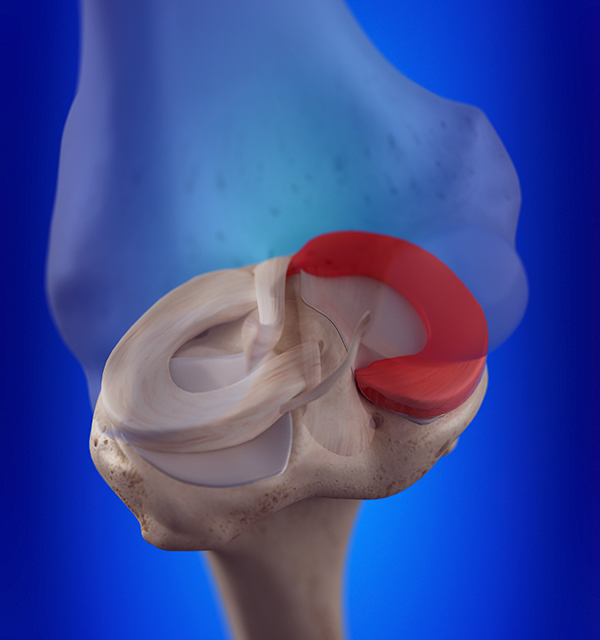
The patient with a meniscal tear that is likely to benefit from surgery more than conservative care is one who developed the onset of symptoms acutely, does not have any arthritis, and who has painful mechanical symptoms of catching or locking. Surgery is an outpatient procedure that is performed arthroscopically, typically through two small “poke-hole” incisions. During the arthroscopy, all of the structures within the knee joint are evaluated and any other abnormal findings are documented and addressed, if indicated. The specific treatment for a meniscal tear is often not determined until the tear can be evaluated at the time of surgery. Given the important functions of the meniscus, efforts are made at the time of surgery to preserve as much of the meniscus as possible, either by repairing the tear or by removing only the torn portion.
Arthroscopic surgery that involves simply removing the torn portion of the meniscus is referred to as partial menisectomy. We know that once the meniscus has torn, there is already a 6-fold increased risk of developing radiographic evidence of arthritis over a 30 month period.1 This suggests that the torn portion of a meniscus is no longer functionally protective to the knee, so by removing only this area and preserving the rest, we are addressing the problem without further impacting the risk of arthritis. The advantages of this procedure include rapid mobility without a brace or weight bearing restrictions and a shorter rehabilitation period, typically returning to full activities after 6 weeks.
Arthroscopic surgery that involves sewing/stitching the meniscus back together is referred to as meniscal repair. The advantages of meniscal repair are maintenance of the meniscal tissue and the advantage of diminishing the risk of degenerative arthritis. The disadvantages include the possibility of recurrent tears, additional post-operative restrictions that often require limitations in weight-bearing for 6 weeks, and a lengthier rehabilitation period, lasting approximately 6 months.
Unfortunately, the meniscus has a relatively poor blood supply, resulting in a limited ability for tears to heal. Because of this fact, only meniscal tears in younger patients with certain tear patterns have historically been selected for an attempted repair. Using traditional techniques, the rate of failure, or lack of meniscus healing following a repair, has typically fallen between 15-30%.2
In recent years, newer surgical techniques and the use of biologic aids, such as platelet-rich plasma (PRP) and stem cells, have yielded improved rates of meniscal healing. Improved surgical instrumentation and suturing techniques have allowed us to repair tears that have been previously considered irreparable. Moreover, by drilling small bone tunnels (bone marrow vents) at the time of meniscal repair, we allow for the egress of mesenchymal stem cells, growth factors, and platelets, all of which coat the meniscal repair and assist in the healing process. Studies have shown this technique to mimic the improved healing rates of around 90% that are observed when meniscus repairs are performed in the setting of an ACL surgery.3,4 Another recent study from The Ohio State University revealed that healing rates of isolated meniscal repairs improved from 77% up to 95% when PRP was injected adjacent to the meniscal repair site during surgery.5
One important factor, independent of the meniscal tear, that will often determine how well patients feel after surgery is the presence or absence of damage to the articular cartilage surfaces. In one study, patients without additional articular cartilage damage reported the results of surgery to be good or excellent 94.8% of the time. However, patients that were found to have articular cartilage damage, in addition to their meniscal tear, reported good or excellent results only 62% of the time.6 If there are any areas of damaged articular cartilage, various treatment techniques can be employed depending on the extent of the damage. Smaller areas of less damage can be debrided (termed chondroplasty). If more specialized treatments are indicated, such as a cartilage transplant, then these small areas of damage may be left alone until further discussion can take place following the surgery.
Although a number of studies have shown that meniscal surgery in the setting of arthritis generally yields no benefit, there are a few notable exceptions. A 2020 level 2 cohort study out of Stanford has revealed that patients with a specific tear pattern (meniscal root tears) in the setting of moderate arthritis experience significantly improved functional outcomes and a lower rate of requiring a total knee replacement (3% vs 33% in the control group over a 4.4 year mean follow-up period).7
At Pro Sport Orthopedics, we are constantly reviewing the latest, cutting-edge treatment options. It is important to recognize that not all choices are appropriate for all patients. However, we strive to provide the best customized course of treatment for each patient and welcome discussions pertaining to all available options.
1. Englund M, Guermazi A, Roemer FW, Aliabadi P, Yang M, Lewis CE, Torner J, Nevitt MC, Sack B, Felson DT. Meniscal tear in knees without surgery and the development of radiographic osteoarthritis among middle-aged and elderly persons: The Multicenter Osteoarthritis Study. Arthritis Rheum. 2009 Mar;60(3):831-9. doi: 10.1002/art.24383.
2. Ardizzone CA, Houck DA, McCartney DW, Vidal AF, Frank RM. All-Inside Repair of Bucket-Handle Meniscal Tears: Clinical Outcomes and Prognostic Factors. Am J Sports Med. 2020 Mar 20:363546520906141. doi: 10.1177/0363546520906141.
3. Feng H, Hong L, Geng XS, Zhang H, Wang XS, Jiang XY. Second-look arthroscopic evaluation of bucket-handle meniscus tear repairs with anterior cruciate ligament reconstruction: 67 consecutive cases. Arthroscopy. 2008 Dec;24(12):1358-66.
4. Dean CS1, Chahla J, Matheny LM, Mitchell JJ, LaPrade RF. Outcomes After Biologically Augmented Isolated Meniscal Repair With Marrow Venting Are Comparable With Those After Meniscal Repair With Concomitant Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2017 May;45(6):1341-1348. doi: 10.1177/0363546516686968. Epub 2017 Feb 1.
5. Everhart JS, Cavendish PA, Eikenberry A, Magnussen RA, Kaeding CC, Flanigan DC. Platelet-Rich Plasma Reduces Failure Risk for Isolated Meniscal Repairs but Provides No Benefit for Meniscal Repairs With Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2019 Jul;47(8):1789-1796. doi: 10.1177/0363546519852616. Epub 2019 Jun 5.
6. Schimmer RC, Brülhart KB, Duff C, Glinz W. Arthroscopic partial meniscectomy: a 12-year follow-up and two-step evaluation of the long-term course. Arthroscopy. 1998 Mar;14(2):136-42.
7. Dragoo JL, Konopka JA, Guzman RA, Segovia N, Kandil A, Pappas GP. Outcomes of Arthroscopic All-Inside Repair Versus Observation in Older Patients With Meniscus Root Tears. Am J Sports Med. 2020 Mar 17:363546520909828. doi: 10.1177/0363546520909828.
Nels Sampatacos, MD
Orthopedic Surgeon and Sports Medicine Specialist


